The leprosy registry’s significance
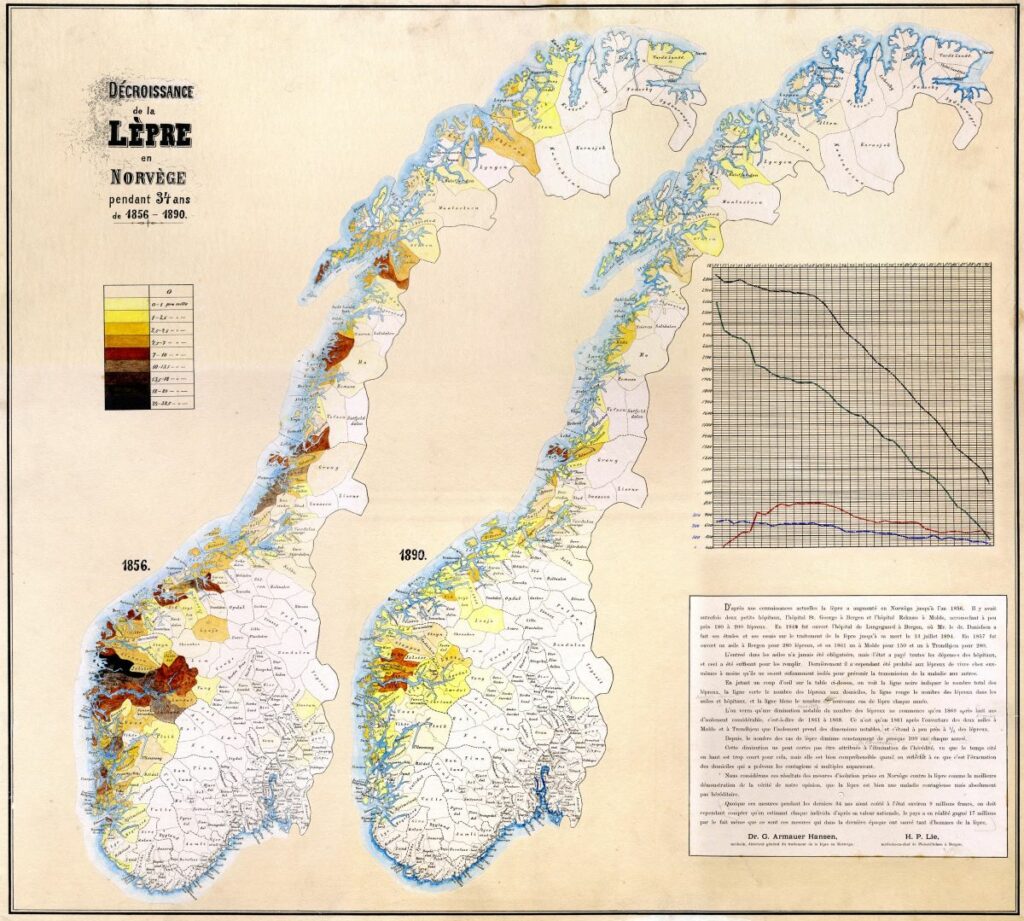
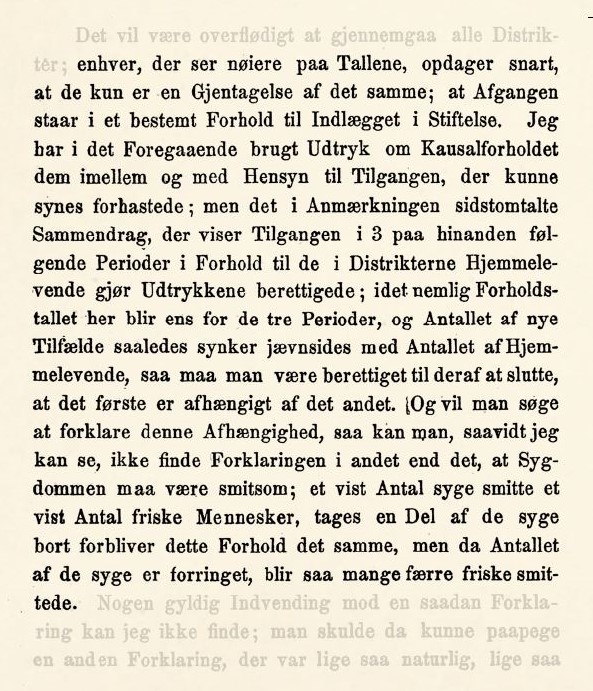
The leprosy registry became a valuable tool for the health authorities in the practical work of preventing the spread of the disease. Since the district medical officers sent in forms at least once a year, the public health issue could be continuously monitored. It enabled the progression and regression of the disease to be tracked in different geographical areas, and different measures to be planned, implemented and assessed. The overview also provided a basis for monitoring and potentially implementing direct interventions for different individuals, such as the hospitalisation of the most severely ill, who were considered most infectious, as it was not possible to institutionalise everyone.
In the latter half of the 19th century, opinion remained divided about what caused leprosy, and there was consequently disagreement about the best way to combat the disease. However, the leprosy registry strengthened the argument that the disease was infectious and that isolation was the most effective measure to prevent its spread. In 1888, medical officer Hansen concluded that, according to statistical data, the measures implemented to prevent the spread of the disease had been successful, i.e. registering those with leprosy, building institutions and isolating the most infectious.
The ability to evaluate the health authorities’ measures by using such a system attracted international attention. The significance of the leprosy registry in combating the disease was clearly expressed at the end of the first International Leprosy Conference in Berlin in 1897. At the conference, the following resolution was adopted: ‘the system of obligatory notification and of observation and isolation, as carried out in Norway, is recommended to all nations with local self-government and a sufficient number of physicians.’
The leprosy registry represented a medical innovation, and the experience gained naturally had an impact on the development of disease registration in Norway. In 1900, tuberculosis registration was introduced, albeit on a smaller scale than the leprosy registry, and for a long time, it only included local registrations. The tradition of patient registries, which started with leprosy and continued with tuberculosis, was then extended to include the registration of non-infectious diseases as well.
Statistics Norway, www.ssb.no